Abstract
Background
Pregnant women with antiphospholipid antibodies (aPLs) or antiphospholipid syndrome have an increased risk for thrombosis. Although a combination of low-dose aspirin and unfractionated heparin (UFH) or low molecular weight heparin (LMWH) are usually prescribed in pregnancy, there is no consensus on optimal dosing of these agents. Despite the use of low-dose aspirin and LMWH, approximately 30% of women with a positive lupus anticoagulant (LA), underlying autoimmune disease, or a previous history of thrombosis have unfavorable outcomes.
Aim
To describe the management and outcomes of women with either aPLs or APS during pregnancy at a university medical center.
Methods
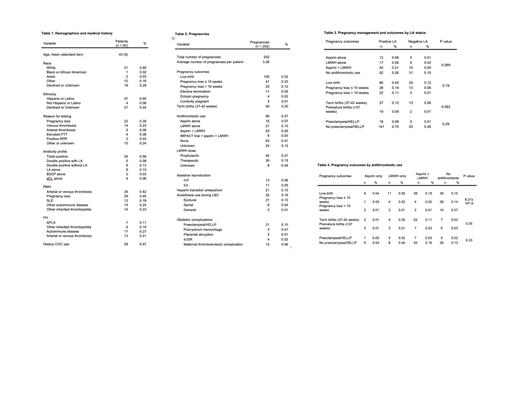
We conducted a retrospective cohort study of pregnant women with either aPLs or APS seen in our hematology clinic in consultation between January 2006 and August 2021. Data collected included demographics, reason for aPLs testing, personal or family history of thrombosis or autoimmune disease, and presence of other thrombophilias. Antiphospholipid antibodies included the LA, anti-cardiolipin (aCL) and anti-beta-2 glycoprotein 1 (ß2GP1) confirmed on two occasions at least 12 weeks apart. Data was collected on antithrombotic agents used during pregnancy, including aspirin, dose of LMWH, UFH and certolizumab. We recorded the following obstetric outcomes: live births, early delivery, fetal loss, early pregnancy loss <10 weeks gestational age (GA), pre-eclampsia, venous thromboembolic events (VTE), arterial thromboembolism (ATE), and post-partum hemorrhage (PPH). We compared management and outcomes in the presence or absence of LA. Statistical comparisons between groups were conducted with the Fisher's exact test.
Results
There was a total of 202 pregnancies in 62 women with 11% of pregnancies achieved with assisted reproductive techniques. The most common reasons for aPLs testing were pregnancy loss (35%), VTE (23%), and ATE (8%). Antiphospholipid antibody profiles consisted of 56% triple positive, 8% positive LA plus either aCL or anti- ß2GP1, 13% positive LA alone and 22% with either double positive aCL and anti- ß2GP1 or single aCL or anti- ß2GP1. Twenty-tree percent of women had an additional inherited thrombophilia (Table 1). Of the 202 pregnancies, 52% resulted in live births, 20% in pregnancy loss <10 weeks, 12% in pregnancy loss >10 weeks, and 28% were either electively terminated, resulted on an ectopic pregnancy, or the outcome was unknown due to lost to follow up. Antithrombotic therapy was used in 47% of pregnancies: 26% used aspirin and LMWH, 10% used LMWH alone, and 7% used aspirin alone (Table 2). In 10% of pregnancies, patients were transitioned to UFH prior to delivery. Pre-eclampsia with or without HELLP syndrome occurred in 10% of pregnancies and maternal thromboembolic complications occurred in 6%. On analysis of outcomes stratified by LA status, there was a trend toward a higher rate of preterm births in the presence of a positive LA (Table 3). The rate of live births was increased with the use of antithrombotic therapy (Table 4).
Conclusion
Patients with antiphospholipid antibodies (aPLs) and antiphospholipid syndrome had elevated rates of complications and adverse outcomes during pregnancy. LA positive status was associated with a trend toward a higher rate of preterm births. Further studies are needed to clarify the factors associated with adverse outcomes and optimal anticoagulation management.
Desancho: Sanofi-Genzyme: Membership on an entity's Board of Directors or advisory committees.
Certolizumab with the hypothesis of improving clinical outocomes

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal